PRESENTATION ON THE IDENTIFICATION OF NEISSERIA GONORRHOEAE IN MEDICAL LABORATORIES
OUTLINE
OTHER IDENTIFICATION TECHINQUES
COMPLICATIONS OF GONORRHOEA
PREVENTION
TREATMENT
CONTROL, RECOMMENDATIONS AND CONCLUSIONS
INTRODUCTION
- The genus Neisseria includes a group of closely related Gram-negative diplococci that are primarily commensal organisms of the mucous membranes of mammals (Knapp, 1988a).
- Several Neisseria spp. are opportunistic pathogens causing disease in immunocompromised hosts.
- Two species, N. gonorrhoeae (the gonococcus) and N. meningitidis (the meningococcus), are important human pathogens.
- Neisseria gonorrhoeae belongs to the genus Neisseria within the family Neisseriaceae
- Neisseria gonorrhoeae, also known as gonococcus (singular), or gonococci (plural), is a species of Gram-negative diplococci bacteria isolated by Albert Neisser in 1879.
- It causes the sexually transmitted genitourinary infection gonorrhea as well as other forms of gonococcal disease including disseminated gonococcemia, septic arthritis, and gonococcal ophthalmia neonatorum.
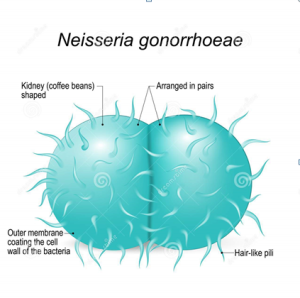
MORPHOLOGY AND STRUCTURE
- Under the microscope, it appears as a gram-negative coccus which is present in pairs (diplococci) with the flattening of the adjacent sides.
- The diameter ranges from 0.6-1 μm.
- The diplococci have kidney/coffee bean shape.
- It is a non-spore forming bacteria and is able to move using twitching motility.
- Gonococci exhib it pili on their surface.
- Pili enhances the binding of the cocci to the mucosal surfaces and promotes virulence by restricting phagocytosis.
- Human red blood cells are agglutinated by piliated gonococci, but not red cells from other mammals.
EPIDEMOILOGY
- Global incidence — The precise global burden of N. gonorrhoeae is difficult to establish because of the lack of diagnostic capability and/or reporting systems in many parts of the world.
- In 2020, the estimate for N. gonorrhoeae was 82.4 million cases.
- The WHO African Region had the highest incidence rate, followed by the South-East Asia region.
- Despite a small decrease in the global incidence of gonorrhea in recent years, the incidence of gonorrhea in the United States has been increasing. In 2020, gonorrhea was the second most common notifiable STI in the United States, with 677,769 reported cases.
PATHOGENESIS
- Gonorrhea is a sexually transmitted disease.
- Gonorrhea is a condition that is essentially limited to humans’ mucus-secreting epithelial cells.
- The first stage in the infection is the adhesion of gonococci to the urethra or other mucosal surfaces.
- For the first attachment, the existence of pili is important.
- As the adhesion is quick and firm, the micturition after exposure offers no protection against infection.
- By the third day following infection, the cocci penetrate into the intercellular spaces and enter the subepithelial connective tissue.
- Gonococci presumably penetrate between columnar epithelial cells.
- Stratified squamous epithelium is comparatively resistant to infection.
- The period of incubation is 2-8 days males, 8-10 days in females and 2-5 days for gonococcal opthalmia neonatorum .
- Gonococci invade the genitourinary tract, eye, rectum, and throat mucous membranes, causing acute suppuration that can lead to tissue invasion; which are followed by chronic inflammation and fibrosis.
VIRULENCE FACTORS
- Being typical gram-negative bacteria, Neisseria gonorrhoeae has thin peptidoglycan layer that is sandwiched between the inner cytoplasmic and outer membrane.
- A true carbohydrate capsule does not enclose the outer surface.
- Gonococci are antigenically diverse and are able to modify their surface structures invitro.
- They likely do so in vivo as well in order to prevent host defense.
- The following are included in the surface structures:
- Pili:
- Por protein (Protein I):
- Opa proteins (Protein II):
- Rmp (Protein III):
- Lipo-oligosaccharide (LOS):
- Other proteins:
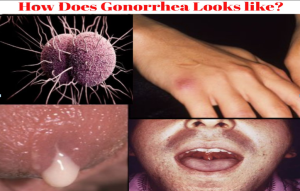
LABORATORY DIAGNOSIS CLINICAL PRESNTATION
- Gonorrhea is caused by the bacteria Neisseria gonorrhoeaeand can be contracted by anyone who has vaginal, anal, or oral sex with someone who has the disease.
- It also can be passed from an infected mother to her baby during childbirth.
- Some men with gonorrhea may have no symptoms at all.
- However, men who do have symptoms may have a burning sensation when urinating, a white, yellow, or green discharge from the penis, and painful or swollen testicles.
- Most women with gonorrhea do not have any symptoms. Even when a woman has symptoms, they are often mild and can be mistaken for a bladder or vaginal infection.
- Symptoms in women can include a painful or burning sensation when urinating, increased vaginal discharge, and vaginal bleeding between periods.
SPECIMENS AND COLLECTION SITES
SPECIMENS:
Specimens in Men:
- urethral discharge
- Exudate from prostatic massage
- Centrifuged urine deposits
- Anal canal – rectal culture in homosexual males.
Specimens in Women:
- Urethral, cervical and rectal specimens
- Throat swab in case of oral sex
Others:
- Blood
- Swabs from skin lesions
- Pus apirated from joint in cases of dessiminated gonococcal ifections
- Conjunctival swab, particularly in the context of neonatal ophthalmia.
Collection sites:
CONDITIONS FOR COLLECTION
- Patients should not pass out urine for at least 2 hours prior to specimen collection.
COLLECTION
- Massage the urethra from proximal to distal to present any discharge
- using a cotton swab, discharge present at the meatus is smeared on a slide and air dried and then placed on an appropriate transport medium
- In the absence of a discharge, retract prepuce using a moistened metal swab with normal saline and inserted 2 to 3 cm inside the urethra and gently rotated once or twice and removed.
- If no slide is made the lab with prepare one from the swab placed in the transport medium
- An air dried smear made at the time of specimen collection is of superior quality.
- High Vaginal swabs (HVS) are not suitable for the isolation of N. gonorrhoeae, Endocervical swabs should be
submitted.
ANALYSIS
–If this is not feasible, specimens should be obtained with swabs impregnated with charcoal and transmitted to the laboratory in the Stuart’s transport medium.
- Direct microscopy:
–Gram staining is performed with a few extracellular species that are typical of gonococcal infection.
–The smear is confirmed as positive, showing characteristic kidney-shaped gram-negative diplococci lying inside polymorphonuclear leucocytes.
–About 95 percent of males infected would develop a positive smear.
–It must be stressed that the diagnosis of gonorrhea by smear analysis in women is inaccurate since some of the typical genital flora has a morphology that is essentially identical.
–The use of fluorescent antibody techniques in the smear identification of gonococci is more sensitive and specific diagnosis by microscopy.
–Culture:
- In acute gonorrhea, cultures can be acquired commonly on chocolate agar or Mueller-Hinton agar incubated at 35-36°C along with 5-10% CO2.
- However, it is best to use a selective medium such as the Thayer-Martin medium in chronic cases where mixed infection is normal and when examining lesions such as proctitis.
- After 24 hours of incubation, the plates are examined and morphology and biochemical reactions identify the growth.
- Incubation of primary isolation plates is continued for 48 hours and the above-mentioned procedures re-examine cultures until any specimen can be negatively reported
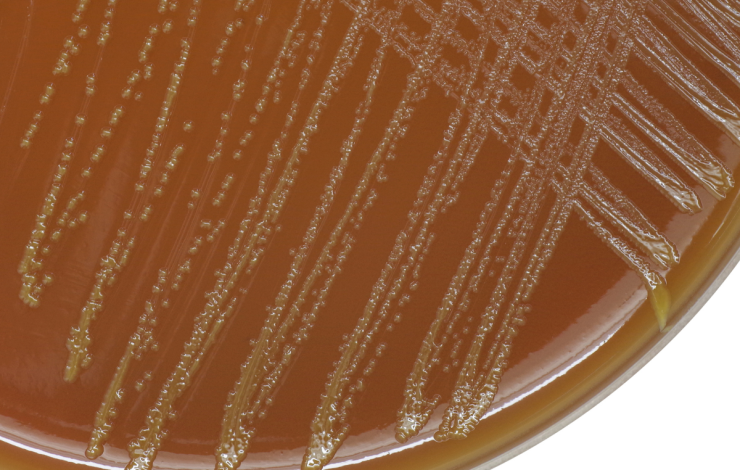
IDENTIFICATION AND COLONIAL MORPHOLOGY
- Gonorrhoeae are preliminarily defined on the basis of the isolation of oxidase-positive, gram-negative diplo-cocci that are selective for pathogenic Neisseria species and grow on chocolate blood agar.
- N. gonorrhoeae is oxidase positive.
- It only ferments glucose with acid.
- In a humid aerobic environment enriched with 5-10% CO2, colonies are thin, round, translucent, convex or slightly umbonate, with finely granular surface and lobate margins after incubation for 24 hours.
- The colonies of Neisseria gonorrhoeae are easily emulsifiable and soft.
- The colonies are larger (1.5-2.5 mm) after 48 hours, often with a crenated margin and an opaque elevated center.
- The transparent, golden-brown pigmentation noticeable in 48 hrs cultures after incubation results from cell autolysis.
- Smear is obtained from the colony and Gram staining is done.
- Gonococci are pair-arranged gram-negative cocci (diplococci) with concave (pear or bean shaped) adjacent sides.
- With gonococcal colonies, substantial variance in size exists and the colony out-line is irregular in most culture media, unlike the circular colonies of N. meningitidis.
- Growth is slower on the Thayer-Martin medium.
- Neisseria gonorrhoeae produces four types of colonies and they are T1, T2, T3, and T4 based on colonial appearance, auto-agglutinability and virulence and was classified by Kellogg.
- T1 and T2: Small brown colonies and possess pili. They are autoagglutinable and virulent strains
- On repeated subcultures, they change to T3 and T4 respectively. They are also known as P+ and P++ respectively.
- T3 and T4: They are larger, granular, non-pigmented colonies and non-piPiliated.
- They form smooth suspensions and are avirulent. They are also named as P-.



Leave a Comment