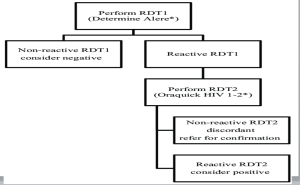
ALGORITHME FOR DIAGNOSING HIV
INTRODUCTION
- Acquired immunodeficiency syndrome (AIDS), caused by infection with the human immunodeficiency virus (HIV), is one of the most prevalent sexually transmitted diseases throughout the world [1].
- Early and rapid identification of HIV infection is crucial for preventing further transmission and facilitating the timely initiation of appropriate care. HIV tests are based on the detection of antibodies to HIV. These are proteins produced by the immune system in response to a foreign substance, such as HIV.
- To avoid situations where people are misdiagnosed with HIV, WHO is encouraging countries with HIV prevalence below 5% to increase the number of tests that are used to confirm an HIV diagnosis. By making this change, countries will be able to ensure HIV testing remains accurate, even as prevalence continues to decline.
- The ideal HIV screening test would correctly identify all HIV-positive and HIV-negative individuals 100% of the time. While many HIV tests are extremely accurate, they do not achieve 100% accuracy.
- Tests always produce a small number of false positive results.
- In settings where very few people have HIV, a higher proportion of reactive results will be false positives.
- A diagnosis of HIV is never made on the basis of a single test result.
DEFINITIONS
- False-Positive Result :
A false-positive HIV result is when a person who does not actually have the virus receives a positive test result.
No test or algorithm can be completely accurate in all cases of HIV infection.
- Specificity:
Is the ability of a test to designate an individual who does not have a disease as negative. Generally, HIV tests have high specificity, meaning that there are few false-positive results and most uninfected individuals are classified as uninfected by the test. If 1,000 uninfected people are tested with an HIV test and 4 have false-positive results, the HIV test’s specificity is 99.6% (996 true negative test results/1,000 HIV uninfected persons tested).
Sensitivity :
Sensitivity refers to a test's ability to designate an individual with disease as positive.A highly sensitive test means that there are few false negative results, and thus fewer cases of disease are missed.
- Positive Predictive Value
The probability that a person with a positive test result is infected with HIV, that is,that they are truly HIV-positive.
- Negative Predictive Value
The probability that a person with a negative test result is not infected with HIV,that is, that they are truly negative
TYPES OF HIV TESTS
- Antibody Tes - 1st Generation: Viral Lysate, IgG Ab detection
- 2nd Generation: Recombinant / Synthetic Peptides, HIV-1/2 IgG Ab detection
- Takes 23 to 90 days to detect HIV after exposure.
- Antigen/Antibody Test
- 3rd Generation: Recombinant / Synthetic Peptides, HIV-1 Ab (Groups M and O), IgG and IgM Ab detection
- 4th Generation: 3rd Gen assay design + HIV-1 p24 Ag detection
Detects HIV-1, Group O, and HIV-2 IgG and IgM antibody
Detects HIV-1 p24 antigen to detect infection about 7 days earlier than third generation tests
- Nucleic Acid Test
PCR
Causes of False-Positive HIV Test Results
Though not limited to the below list, false positive HIV test results can occur due to:
Technical issues
o Specimen mix-up
o Mislabelling
o Improper handling
o Misinterpretation of a visually read rapid test result (Point of Care)
Biological causes ;
o Participation in an HIV vaccine study
o Autoimmune disorders (ex. Lupus and rheumatoid arthritis )
o Recent flu vaccine or gamma-globulin
o Cross reactive antibodies that may be present following a blood transfusion or pregnancy
o Hypergammaglobulinemia related to another condition, such as hematological malignancy, liver cirrhosis or hepatitis
o Other medical conditions or infections
ALGORITHME FOR HIV TESTING IN CAMEROON
WHO Recommendations For HIV Testing Strategies
- Western blotting and line immunoassays should not be used in national HIV testing strategies and algorithms.
- Dual HIV/syphilis rapid diagnostic tests (RDTs) can be the rst test in HIV testing strategies and algorithms in antenatal care settings.
- In response to changes in the HIV epidemic, WHO recommends countries use three consecutive reactive tests to provide an HIV- positive diagnosis.
- Testing strategies should use tests serially, not in parallel and should not use a tiebreaker to rule- in HIV infection.
- WHO recommends that all HIV testing algorithms use a combination of RDTs and/or enzyme- immunoassays (EIAs) to achieve at least 99% positive predictive value and use a combination of tests with ≥99% sensitivity and ≥98% specicity. WHO does not recommend the use of nucleic acid testing techniques within HIV testing algorithms for individuals ≥18 months of age.
- The rst test in an HIV testing strategy and algorithm should have the highest sensitivity, followed by a second and third test of the highest specicity. Algorithms should be validated and verified to ensure high- quality and accurate testing.
-All people newly diagnosed with HIV should be retested to verify their HIV status prior to starting ART.
STATISTICS

RECOMMENDATIONS
To avoid situations where people are misdiagnosed with HIV, WHO is encouraging countries with HIV prevalence below 5% to increase the number of tests that are used to confirm an HIV diagnosis.
WHO advices that patients are concoiled before the undergo an HIV test before test and after results.

Leave a Comment